Last updated on June 8th, 2023 at 10:17 am
Ulcerative colitis vs. Crohn’s — if you’ve been diagnosed with one of these chronic inflammatory bowel diseases, you may be wondering how they differ.
While they do share some similarities, there are important contrasts between the two conditions that affect their treatment and management.
In this comparative guide, we’ll explore the key features of ulcerative colitis and Crohn’s disease, including their symptoms, causes, diagnosis, and treatment options.
We hope you gain a deeper understanding of these disorders and become better equipped to navigate your journey towards effective management and optimal health.
Ulcerative Colitis and Crohn’s Disease: The Basics
Let’s begin by comparing ulcerative colitis and Crohn’s disease:
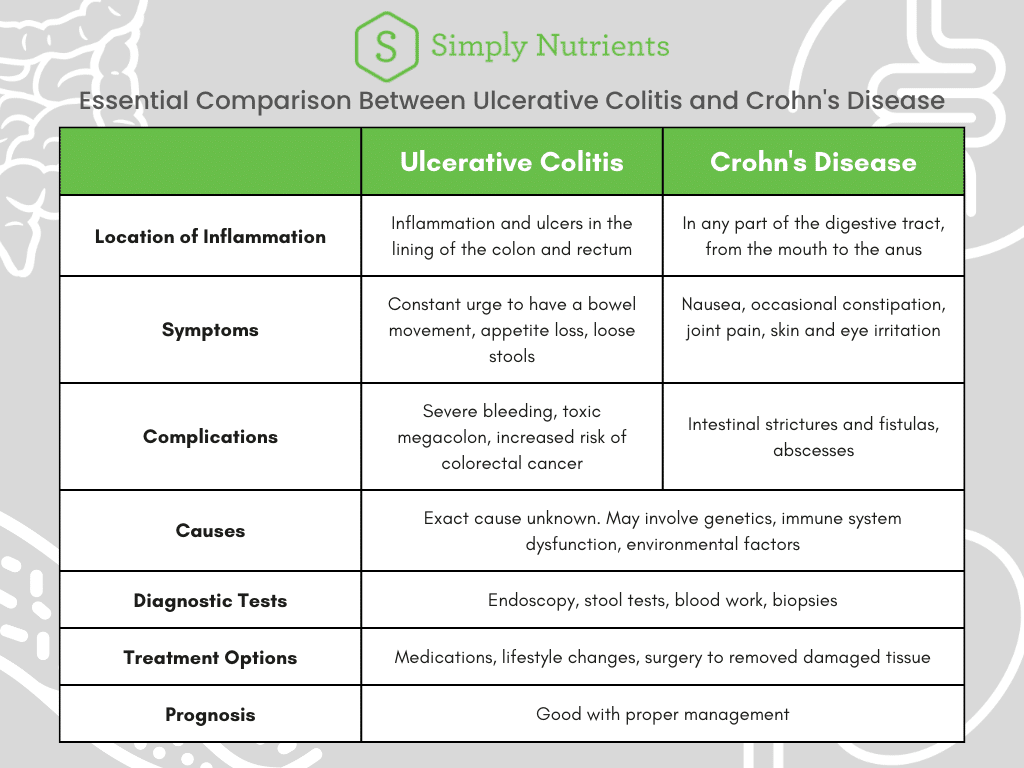
While both of these conditions fall under the umbrella of inflammatory bowel disease, they have distinct differences in their location of inflammation, indicators, and potential complications.
Both disorders disrupt your body’s ability to digest food, absorb nutrients, and eliminate waste. These lifelong conditions can also cause acute periods of active symptoms and other phases without any discomfort.
By understanding these differences, individuals diagnosed with the diseases can work with their healthcare providers to develop an appropriate treatment plan and reduce their discomfort effectively.
Pearl of wisdom: In addition to medications and dietary changes, you could benefit from taking supplements that address compromised gut function to manage your symptoms and improve your overall wellness.
What Is Ulcerative Colitis?
Ulcerative colitis causes inflammation and ulcers in the mucosa and submucosa of the colon and rectum. Having the chronic condition results in a variety of uncomfortable symptoms, such as abdominal pain, rectal bleeding, and the constant urge to have bowel movements.
It typically begins in the rectum and spreads up the colon in a continuous pattern. There are three types of ulcerative colitis based on location:
- Ulcerative proctitis: Bowel inflammation is limited to the rectum. This is the mildest form of ulcerative colitis.
- Left-sided colitis: Affects the descending colon and rectum.
- Extensive colitis: Inflammation of the entire colon.
The severity and frequency of ulcerative colitis symptoms vary widely amongst individuals, and they may flare up periodically before going into remission.
What Is Crohn’s Disease?
Crohn’s disease is another type of inflammatory bowel disease that affects any part of the digestive tract from the mouth to the anus. This swelling causes discomfort, like abdominal pain, diarrhea, and weight loss.
Unlike ulcerative colitis, Crohn’s disease can cause inflammation that isn’t continuous, and may involve all layers of the intestinal wall. It also doesn’t only occur in the digestive system, and can affect the skin, eyes, joints, and liver.
Comparing These Inflammatory Bowel Diseases
While both conditions involve inflammation of the digestive system, there are important differences between them that affect the way they are diagnosed and treated.
In the following few sections, we’ll take a closer look at the symptoms, causes, and management options for ulcerative colitis and Crohn’s disease.
Symptoms
Here’s a table comparing the common and different symptoms of ulcerative colitis and Crohn’s disease:
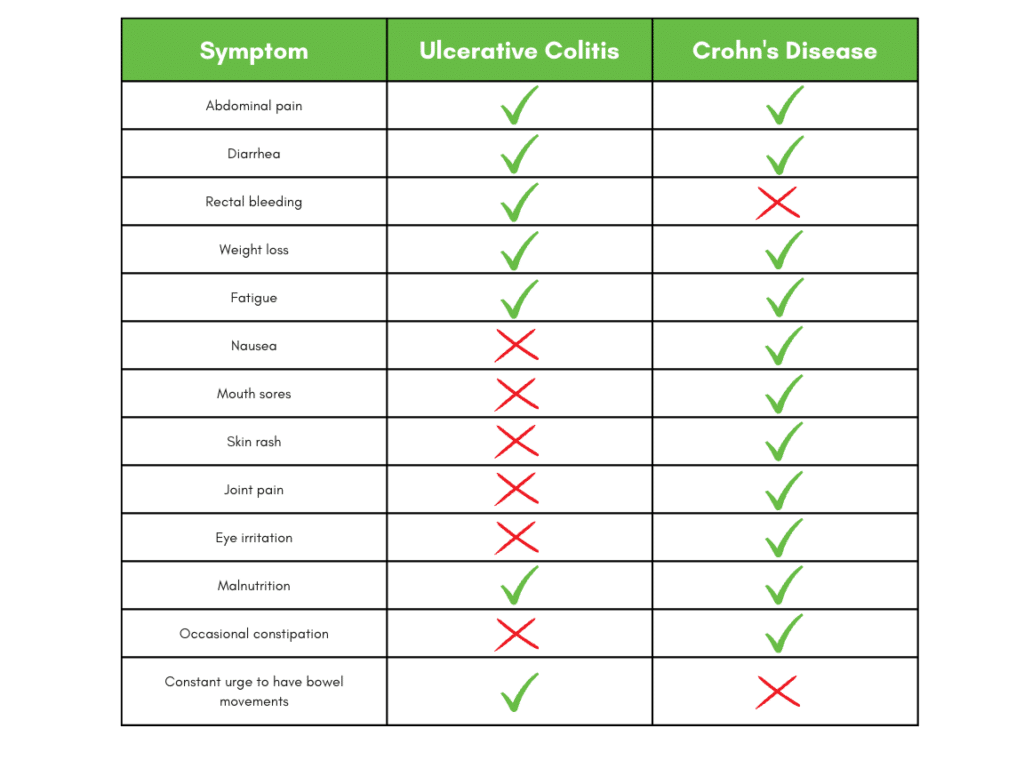
Only your doctor can determine which inflammatory bowel disease you may have, so pay close attention to your indicators in order to describe them to your specialist.
Your diagnosis is usually obvious to a gastroenterologist, but in some cases you may exhibit the features of both disorders. This condition is called indeterminate colitis and affects approximately 10% of people with inflammatory bowel disease according to UCLA.
Causes
Researchers don’t yet know the exact causes of ulcerative colitis and Crohn’s disease, but they believe a combination of factors may contribute to their development [1].
One theory is that an abnormal immune response plays a role [2, 3]. In people with ulcerative colitis and Crohn’s disease, the body’s defense system mistakenly attacks healthy cells in the digestive tract, leading to inflammation and damage to the intestinal lining.
Genetic factors may also play a part, as inflammatory bowel diseases tend to run in families [4].
Environmental triggers, such as diet and stress, may also contribute to the development of ulcerative colitis and Crohn’s disease [5].
Some studies suggest that eating large amounts of sugar, refined carbohydrates, and saturated fats may increase the risk of developing these conditions [6, 7, 8].
Additionally, exposure to certain viruses, bacteria, or pollutants may trigger an immune response that leads to inflammation in the digestive tract [9, 10].
Important note: While these factors may increase the chances of developing ulcerative colitis or Crohn’s disease, not everyone exposed to them will develop the disorders. It’s possible that other, unidentified elements may play a role.
Diagnosis
The diagnostic process usually begins with a thorough medical history and physical exam, this can help your doctor identify any risk factors and symptoms that suggest ulcerative colitis or Crohn’s disease.
Your healthcare provider may also order blood tests to look for signs of inflammation, infection, or anemia.
Imaging studies, like an endoscopy, visualize the inside of the digestive system and identify any inflammation, ulceration, or other abnormalities. These procedures involve inserting a small camera into the body.
For ulcerative colitis, practitioners only insert the endoscope into the anus. There are two types of examination:
- Sigmoidoscopy: The doctor examines your rectum and lower colon for the extent of inflammation in the area.
- Total colonoscopy: Involves checking the entire colon.
Should your healthcare provider suspect you have Crohn’s disease, they may perform:
- Colonoscopy: Your doctor inserts the camera through the anus to examine the colon.
- Upper endoscopy: The flexible tube goes into your mouth, down your esophagus, into your stomach, and enters the first part of your small intestine.
For both conditions, your specialist may require additional tests like stool samples or biopsies to confirm your diagnosis and rule out other illnesses with similar indicators.
Complications
The complications of ulcerative colitis and Crohn’s disease can differ, depending on the location and extent of inflammation.
Those that are more common in ulcerative colitis include:
- Severe bleeding: Ulcers that form in the colon lining may bleed.
- Toxic megacolon: A rare, but life-threatening complication, when the colon becomes severely inflamed and dilated, leading to a risk of perforation or sepsis.
- Increased risk of colon cancer: Patients with ulcerative colitis have a higher risk of developing colon cancer, especially if they’ve had the disease for many years or their entire colon is affected [11].
The following complications are more prevalent in Crohn’s disease:
- Intestinal strictures: The walls of the intestines thicken and narrow, leading to blockages.
- Fistulas: Abnormal connections form between different parts of the intestine, or between the intestine and other organs.
- Abscesses: Pockets of pus can form in the wall of the intestine or nearby tissue.
Treatment Options
The treatment for both conditions aims to reduce inflammation, relieve symptoms, and prevent complications. Options may vary depending on the severity of the disease and your overall health.
A balanced diet can help manage symptoms, provided you avoid any trigger foods that may worsen irritation [12].
Managing stress and getting regular exercise may also help reduce any discomfort [13].
In severe cases of ulcerative colitis or Crohn’s disease, surgery may be necessary to remove the affected part of the intestine or repair a fistula.
Several classes of medications can treat ulcerative colitis and Crohn’s disease, including anti-inflammatories, immunosuppressants, and biologic therapies.
In recent years, there has also been increasing interest in using supplements to support gut health and reduce symptoms in individuals with inflammatory bowel diseases.
One such supplement is MegaMucosa, which contains a blend of nutrients and immunoglubulins that could help strengthen the intestinal lining and promote the growth of beneficial bacteria in the digestive tract..

By doing so, MegaMucosa may help to reduce inflammation and improve symptoms like diarrhea, cramping, and bloating.
Prognosis
Both conditions are chronic and may have a significant impact on your quality of life. However, with proper medical management, many people with ulcerative colitis and Crohn’s disease can control their symptoms and achieve long-term remission.
Work closely with your specialist to develop a treatment plan and monitor your health regularly.
Take Control of Your Inflammatory Bowel Disease
We understand that an inflammatory bowel disease diagnosis can be scary and want you to know that you’re not alone on your journey. Don’t hesitate to contact us for more information on how to manage your condition and live a more fulfilling life.
Simply Nutrients’ team of experts dedicates itself to helping our customers and providing personalized guidance and advice on your unique situation. Together, we can help you take control of your condition and improve your well-being.
Resources
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4945988/
[2] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5757119/#:~:text=Core%20tip%3A%20It%20is%20now,that%20the%20mechanism%20remains%20unclear.
[3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8780689/
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4172738/
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4716022/
[6] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4213135/
[7] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8517080/
[8] https://pubmed.ncbi.nlm.nih.gov/21468064/
[9] https://bmjopengastro.bmj.com/content/8/1/e000573
[10] https://journals.lww.com/environepidem/FullText/2019/10001/Air_pollution_and_greenness,_and_their_associated.337.aspx
[11] https://www.mdanderson.org/cancerwise/does-ulcerative-colitis-affect-your-colorectal-cancer-risk.h00-159462423.html#:~:text=Having%20ulcerative%20colitis%20doesn’t,or%20extend%20throughout%20the%20colon.
[12] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4843040/
[13] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4022156/
NOTHING IN THIS WEBSITE IS INTENDED AS, OR SHOULD BE CONSTRUED AS, MEDICAL ADVICE. ANY HEALTHCARE AND/OR NUTRITIONAL MATERIAL CONTAINED IN THIS WEBSITE IS FOR CONSUMER INFORMATIONAL AND EDUCATIONAL PURPOSES ONLY. SUCH MATERIAL IS NOT INTENDED AS MEDICAL ADVICE FOR CONDITIONS OR TREATMENT, NOR IS IT INTENDED AS A SUBSTITUTE FOR A MEDICAL EXAMINATION BY A HEALTHCARE PROFESSIONAL. CONSUMERS SHOULD CONSULT THEIR OWN HEALTH CARE PROFESSIONALS FOR INDIVIDUAL MEDICAL RECOMMENDATIONS.
- Magnesium Threonate: An Honest Buying Guide for Health Enthusiasts - March 21, 2024
- Magnesium Citrate Vs Glycinate: 5 Key Differences And Benefits - March 14, 2024
- How to Pick the Best Magnesium Glycinate Supplement for You - March 7, 2024